Medhavi Sharma 1, Stephen W. Leslie 2
In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.
2023 Nov 18.
Affiliations Expand
- PMID: 35201719
- Bookshelf ID: NBK578191
Free Books & Documents
Excerpt
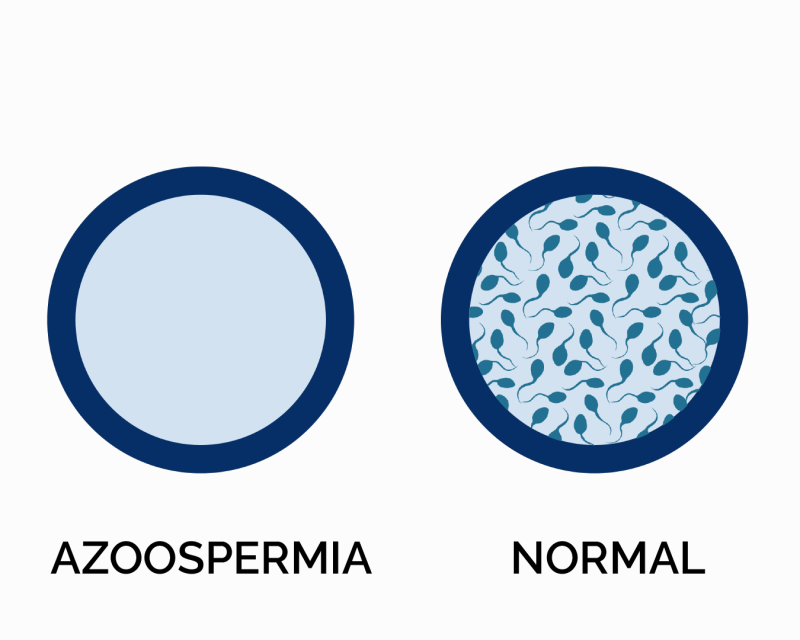
Male factors are crucial contributors to infertility amongst infertile couples. The overall incidence of infertility accounts for nearly 15% of the total population. Male infertility in its most severe form is known as azoospermia. Azoospermia is defined as the complete absence of spermatozoa in 2 separate centrifuged semen specimens, while aspermia is the total lack of ejaculate. Azoospermia affects nearly 1% of the male population and about 10% to 15% of all males with infertility. Many untreatable testicular disorders result in azoospermia, the most severe form of male infertility.
Azoospermia can be subdivided into pre-testicular, testicular, or post-testicular causes (see Table 1. Etiologic Classification According to Pre-testicular, testicular, and Post-testicular Causes). Based on the presence or absence of obstruction of the ducts or vas deferens, azoospermia can be classified into obstructive azoospermia (OA) and nonobstructive azoospermia (NOA). It is essential to differentiate between Oa and NOA, ie, primary testicular failure. With advanced assisted reproductive technologies, various fertility options are available for couples having difficulties in conception due to male infertility, even azoospermia.
Amongst azoospermic males, 40% will have OA. OA causes include congenital bilateral absence of the vas deferens, obstruction of ejaculatory and epididymal ducts, atresia of the seminal vesicles, various infections of the genitourinary tract resulting in obstruction or pelvic and inguinal procedures leading to a complete blockage such as a bilateral vasectomy.
In OA, spermatogenesis is often normal. Therefore, treatment options for OA often include the surgical correction of the blockage in addition to other assisted reproductive techniques.
The majority of azoospermic men, about 60%, will have NOA, making it the most common type of azoospermia. NOA is most often due to severe defects in spermatogenesis, which are frequently due to primary testicular failure or dysfunction. It can also result from dysfunction of the pituitary or hypothalamus. The exact pathology of NOA is often idiopathic. Advanced assisted reproductive techniques can often treat NOA (primary testicular failure).
Testicular biopsies of patients suffering from severe spermatogenic failure often show various areas of normal spermatogenesis. These sperm can be retrieved using testicular sperm extraction (TESE) or testicular sperm aspiration (TESA) techniques and used in advanced assisted reproductive techniques such as intracytoplasmic sperm injection (ICSI). Sperm retrieved from the testes in these ways and used for in vitro fertilization with ICSI generally results in healthy offspring.
Healthcare professionals face many challenges in providing care to infertile men with spermatic failure. Diagnostic modalities used for patients with azoospermia are hormonal assessment, biomarkers in semen, ultrasonography, testicular biopsy, and vasography. The best tool for diagnosing distal male reproductive system obstruction is transrectal ultrasound.
Copyright © 2025, StatPearls Publishing LLC.
Conflict of interest statement
Disclosure: Medhavi Sharma declares no relevant financial relationships with ineligible companies.
Disclosure: Stephen Leslie declares no relevant financial relationships with ineligible companies.
Sections
- Continuing Education Activity
- Introduction
- Etiology
- Epidemiology
- Pathophysiology
- History and Physical
- Evaluation
- Treatment / Management
- Differential Diagnosis
- Prognosis
- Complications
- Deterrence and Patient Education
- Pearls and Other Issues
- Enhancing Healthcare Team Outcomes
- Review Questions
- References
Similar articles
- Genetic profiling of azoospermic men to identify the etiology and predict reproductive potential.Cheung S, Ng L, Xie P, Kocur O, Elias R, Schlegel P, Rosenwaks Z, Palermo GD.J Assist Reprod Genet. 2024 Apr;41(4):1111-1124. doi: 10.1007/s10815-024-03045-5. Epub 2024 Feb 26.PMID: 38403804Free PMC article.
- Ultrasonographic caput epididymis diameter is reduced in non-obstructive azoospermia compared with normozoospermia but is not predictive for successful sperm retrieval after TESE.Pezzella A, Barbonetti A, D’Andrea S, Necozione S, Micillo A, Di Gregorio A, Francavilla F, Francavilla S.Hum Reprod. 2014 Jul;29(7):1368-74. doi: 10.1093/humrep/deu092. Epub 2014 May 7.PMID: 24812316
- Microdissection testicular sperm extraction (micro-TESE) in men with infertility due to nonobstructive azoospermia: summary of current literature.Achermann APP, Pereira TA, Esteves SC.Int Urol Nephrol. 2021 Nov;53(11):2193-2210. doi: 10.1007/s11255-021-02979-4. Epub 2021 Aug 19.PMID: 34410586Review.
- Clinical outcomes and development of children born to couples with obstructive and nonobstructive azoospermia undergoing testicular sperm extraction-intracytoplasmic sperm injection: A comparative study.Tsai YR, Huang FJ, Lin PY, Kung FT, Lin YJ, Lan KC.Taiwan J Obstet Gynecol. 2015 Apr;54(2):155-9. doi: 10.1016/j.tjog.2014.03.005.PMID: 25951720
- Non-Obstructive Azoospermia and Intracytoplasmic Sperm Injection: Unveiling the Chances of Success and Possible Consequences for Offspring.Majzoub A, Viana MC, Achermann APP, Ferreira IT, Laursen RJ, Humaidan P, Esteves SC.J Clin Med. 2024 Aug 21;13(16):4939. doi: 10.3390/jcm13164939.PMID: 39201081Free PMC article.Review.
References
- Aziz N. The importance of semen analysis in the context of azoospermia. Clinics (Sao Paulo) 2013;68 Suppl 1(Suppl 1):35-8. – PMC – PubMed
- Esteves SC, Miyaoka R, Agarwal A. An update on the clinical assessment of the infertile male. [corrected]. Clinics (Sao Paulo) 2011;66(4):691-700. – PMC – PubMed
- Esteves SC, Agarwai A. The azoospermic male: current knowledge and future perspectives. Clinics (Sao Paulo) 2013;68 Suppl 1(Suppl 1):1-4. – PMC – PubMed
- Jarvi K, Lo K, Grober E, Mak V, Fischer A, Grantmyre J, Zini A, Chan P, Patry G, Chow V, Domes T. The workup and management of azoospermic males. Can Urol Assoc J. 2015 Jul-Aug;9(7-8):229-35. – PMC – PubMed
- Jarow JP, Espeland MA, Lipshultz LI. Evaluation of the azoospermic patient. J Urol. 1989 Jul;142(1):62-5. – PubMed
Show all 96 references
Publication types
Related information
LinkOut – more resources
- Full Text Sources
- Medical